As you face the daily challenges of life, you may find your thoughts clouded by feelings of sadness and hopelessness. The connection between depression and central nervous system (CNS) depressants is one that deserves thorough understanding. Moving forward with knowledge empowers you to make informed choices regarding mental health and substance use.
What Are CNS Depressants?
Definition and Effects
CNS (central nervous system) depressants are a category of drugs that slow down brain activity. They can produce a sedating effect, making you feel relaxed or sleepy. Common examples include benzodiazepines like Xanax or Valium, barbiturates, and sleep medications. If you or a loved one is struggling with CNS depressant dependency issues, call us at (617) 917-3485 today or reach out online.
Link to Depression
While CNS depressants can provide short-term relief from anxiety or insomnia, long-term use increases the risk of developing depression. They can disrupt normal brain chemistry and emotion regulation over time. Stopping them abruptly after dependence also triggers rebound anxiety and depressive symptoms.
Risks and Precautions
Using CNS depressants, especially with other substances like alcohol, can dangerously suppress breathing and heart rate. Only take them as prescribed to avoid addiction, overdose, or worsening mental health issues like depression.
Effects of CNS Depressants
Physical Impairments
CNS depressants can produce profound drowsiness, dizziness, poor concentration, and slurred speech. You may experience issues with coordination and slow reaction times that impact daily functioning and increase risks of accidents or injuries. Long-term use can also lead to respiratory depression, coma or death.
Psychological Effects
These drugs can induce feelings of apathy, confusion, and disorientation. Prolonged misuse may contribute to developing depression, anxiety disorders, or exacerbating existing mental health conditions. You could experience mood swings, loss of motivation, and struggle to find pleasure in previously enjoyable activities.
Dependency and Addiction
CNS depressants have a high potential for abuse and addiction, both physical and psychological. With regular use, tolerance develops rapidly requiring higher doses to achieve the desired effects. Abruptly stopping can trigger severe withdrawal symptoms like insomnia, seizures, and delirium tremens in chronic users. Some people require an acute detox program to assist in safely and successfully tapering off these medications.
Connection Between CNS Depressants and Depression
Increased Risk
CNS depressants, such as opioids, benzodiazepines and barbiturates, can put you at a significantly higher risk of developing depression or worsening existing symptoms. According to a study by the National Institute of Mental Health, individuals who misuse prescription sedatives are nearly twice as likely to experience major depressive episodes.
Brain Chemistry Imbalance
These substances work by slowing brain activity, which can disrupt the delicate balance of neurotransmitters like serotonin, dopamine and norepinephrine. This imbalance can contribute to feelings of sadness, hopelessness and anhedonia – hallmarks of clinical depression.
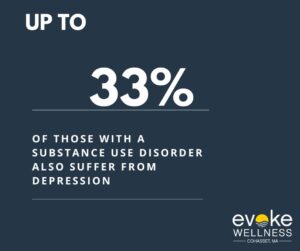
Substance Abuse Comorbidity
Furthermore, there is a strong link between substance abuse disorders and major depression. Up to 33% of those with a substance use disorder also suffer from depression, according to the Anxiety and Depression Association of America. This dual diagnosis complicates treatment and recovery. Thankfully, there are specific dual diagnosis treatment programs tailored toward combatting the two interlinked afflictions.
Signs of CNS Depressant Abuse
Physical Symptoms
Be alert for slurred speech, lack of coordination, and drowsiness. You may notice constricted pupils, shallow breathing, and involuntary eye movements. Over time, abuse leads to weight fluctuations and disrupted sleep patterns.
Mental Changes
Depressant abuse can cause confusion, impaired memory, and difficulty concentrating. Mood swings are common, swinging between anxiety and euphoria. In severe cases, you may experience hallucinations or delusions.
Behavioral Red Flags
Watch for reckless behavior, like erratic driving or risky sexual activity. Social withdrawal, lies, and secretive actions often accompany addiction. You may struggle with work, school, or relationships.
Early recognition of these physical, mental, and behavioral signs is crucial. Seek professional help if you or a loved one exhibit multiple symptoms of CNS depressant abuse.
Treatment Options for CNS Depressant Addiction and Depression
Intensive Inpatient Rehab Programs
For severe CNS depressant addiction and co-occurring depression, intensive inpatient programs provide 24/7 medical supervision and therapy. In these residential settings, you undergo detoxification, behavioral counseling, and holistic mind-body healing approaches. The highly structured environment removes access to substances while equipping you with relapse prevention skills.
Outpatient Rehab Programs
After completing an inpatient program or for milder cases, outpatient rehab allows you to live at home while receiving treatment. Through regular counseling sessions, support groups, and medication management if needed, you learn to manage cravings and address the root causes of addiction and depression in your daily environment.
Medication-Assisted Treatment
Certain medications can help alleviate withdrawal symptoms and cravings during detox from CNS depressants. Medication-Assisted Treatment uses counseling and behavioral therapies in combination with medication for the most optimal treatment. Anti-depressants or mood stabilizers may also be prescribed to manage co-occurring depression. However, medication should always be combined with behavioral therapies for a comprehensive treatment approach.
With a range of evidence-based treatment options available, overcoming CNS depressant addiction and depression is possible with professional support and a commitment to recovery. Early intervention increases the chances of lasting sobriety and improved mental health.
FAQ: How Do CNS Depressants Affect Depression Symptoms?
Short-Term Effects
CNS depressants like alcohol, benzodiazepines and barbiturates can provide temporary relief from depression symptoms. They slow brain activity, creating a calming effect that can reduce feelings of anxiety and agitation. However, this relief is short-lived as the effects wear off.
Rebound Symptoms
After the initial calming period, many users experience a “rebound” effect where depression symptoms return more intensely. This cycle of uplifting highs followed by crushing lows can actually worsen depression over time.
Dependence and Withdrawal
With continued use, the brain becomes dependent on CNS depressants to function normally. Stopping suddenly can trigger severe withdrawal effects like insomnia, anxiety, tremors and seizures – all of which exacerbate depressive states.
Long-Term Impacts
Chronic depressant abuse alters brain chemistry in ways that increase risks for clinical depression and suicidal thoughts. It damages neurotransmitter systems and shrinks areas of the brain that regulate mood. This can make depressive episodes more frequent and harder to treat.
Conclusion
As we have discussed, the connection between CNS depressants and depression is complex but important to understand. While these drugs may seem to provide temporary relief, the statistics show they can exacerbate depression over time. We all face challenges with mental health, but there are healthier long-term solutions. With compassion for those struggling with depression, education about the risks of CNS depressants, and access to alternative treatments, we can work together to turn the tide. Though the path is difficult, recovery is possible, and we each have a role to play in supporting those who need it most. There is hope, if we choose to walk in light.
Begin Your Journey with Evoke Wellness at Cohasset
If you or a loved one is considering treatment, Evoke Wellness at Cohasset invites you to contact us. Our compassionate team is ready to answer your questions, discuss your needs, and help you take the first steps toward recovery. In Cohasset, you’ll find more than just a treatment program – you’ll discover a community dedicated to your wellness and success. Together, let’s embrace the journey to recovery and the promise of a new beginning. Call us at 866.931.6429 today or reach out online.