You don’t have to be spiraling to be in trouble. High-functioning opioid use sneaks under the radar—wrapped in productivity, responsibility, and that stubborn belief you’re still “fine.” But if you’re reading this, a part of you already suspects it’s more than just a habit. This isn’t judgment. It’s a checkpoint—a chance to see the cracks before they widen.
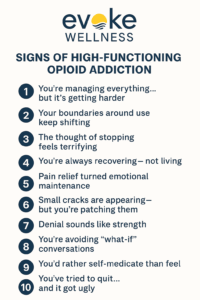
1. You’re Managing Everything… But It’s Getting Harder
From the outside, you’re a poster of normalcy. Deadlines met, meetings hosted, responsibilities upheld. But lately, something’s off. The effort to maintain this façade has grown heavier. Mornings feel like slogging through molasses; evenings are restless avalanches of thoughts you can’t turn off. Life still looks “good”—on paper. But behind the scenes, it’s harder to keep everything from sliding.
High-functioning doesn’t mean immune. In fact, it often means the damage stays silent for longer.
2. Your Boundaries Around Use Keep Shifting
You had rules—clear ones. “Only after work.” “Only on weekends.” “Just when it’s bad.” But those lines keep shifting. You rationalize the exceptions easily. “Just this once.” “I deserve it today.” And before you know it, those exceptions form a pattern. That negotiation isn’t habit—it’s your brain lit up by dependency.
Each rationalization is a thread, pulling you deeper under the surface.
3. The Thought of Stopping Feels Terrifying
Habits don’t scare you. Cravings do. Big difference. If the idea of stopping makes your heart race, your stomach knot, or if you’ve tried to quit and it turned ugly—this isn’t optional use. It’s chemical dependence. Withdrawal isn’t weakness; it’s biology. And opiod addiction treatment exists precisely because your brain and body need a safe reset.
4. You’re Always Recovering—Not Living
Weekends aren’t for fun; they’re for rebooting. You’re exhausted but wired. Moody yet hollow. Life feels like a constant push against gravity, against your own body’s signals to slow down. This chronic cycle isn’t normal; it’s a body under siege. If you’ve lost track of days or find yourself spending your free time just to feel human again, that’s no longer sustainable.
5. Pain Relief Turned Emotional Maintenance
Your journey might’ve started with physical pain—and maybe you needed those prescriptions. But if you’re now turning to pills to handle bad moods, social anxiety, boredom, or low-grade grief, that’s a signal. Emotional regulation isn’t why prescriptions exist. When opioids shift to managing your feelings more than your pain, you’re crossing a line into problem territory.
6. Small Cracks Are Appearing—But You’re Patching Them
Once, you prided yourself on consistency. You were reliable. But lately: missed emails, snapped comments, fuzzy memory. You’re still functioning—but there are fractures, and they’re growing. You don’t have to collapse to need support. You just need clarity.
Staying functional while masking vulnerability is exhausting—and risky.
7. Denial Sounds Like Strength
You tell people, “I’ve got it handled,” because that’s your skill—handling. But lately, handling feels more like spinning plates. You might say, “It’s not that bad,” while scanning for the pills that feel inevitable. Denial isn’t resilience. It’s a shield against fear. And it’s a sign that the coping strategy is wearing thin.
8. You’re Avoiding “What-If” Conversations
Deep down, you know people are noticing. Maybe it’s in their silence, their hesitation, or the subtle distance. You avoid their looks, change the subject, or disappear from social plans. You can’t bear the question: “Are you okay?” Because you don’t know the answer—and you’re afraid of the truth. That emotional isolation is a red flag. Connection helps prevent crisis. Isolation heightens it.
9. You’d Rather Self-Medicate Than Feel
You’re excellent at self-care rituals—workouts, healthy meals, weekend plans. But underneath those routines, opioids are the reason you’re even doing them. They’re not complements. They’re coping tools. When the line between self-care and self-medication blurs, you’re no longer just managing—you’re suppressing.
10. You’ve Tried to Quit… And It Got Ugly
Maybe you tried switching to Tylenol, cutting back, or skipping a dose. Then the tremors started. Your sleep tanked. Your mood unraveled. You couldn’t stop. That physical reaction? It isn’t shame, guilt, or moral failure. It’s dependency. And it means your body has a voice—and it’s screaming that things need to change.
Why Treatment Doesn’t Mean “Rock Bottom”
Your life doesn’t have to crumble for treatment to be successful. In fact, seeking help early means less damage to your relationships, your health, your career—and your self-respect.
At Evoke Wellness in Cohasset, MA, our Prescription Drug Rehab Program in Massachusetts is designed for those who may appear high-functioning on the outside but feel unmanageable inside. We understand the mask. You don’t have to lose everything to deserve care. You just need to want something better than grinding through life.
How Opioid Addiction Treatment Supports You
Early Intervention = Faster Recovery
The sooner you recognize use is more than “okay,” the less damage we have to undo.
Personalized Plans
You’re not a stereotype—you’re you. Treatment is tailored to your physical, emotional, and life context.
Medical and Emotional Support
From medical detox to cognitive work, you’ll have tools—and you don’t have to do it alone.
Reintegration Skills
We help build routines that restore energy and agency—so you don’t just survive; you thrive.
A Metaphor That Hits Home
Imagine your mind is an old car engine. You keep dumping oil into it—not because it needs it, but because that sound of performance feels good. Eventually, the oil sensor breaks. The engine heats up. You can’t tell how much is too much anymore. That car runs—but it’s burning. Treatment? That’s the professional mechanic who not only cools the engine but fixes the sensor so you stop pouring in what hurts you.
Embrace the Question: What If You Could Breathe Again?
You might not be ready to step off a cliff to ask for help. You don’t have to. But you can take the handrail. You can sit with the thought: “What if this is my exit ramp?” This isn’t about blame. It’s about choice. You get to decide which line you draw—for your sanity, your relationships, your life.
If you’re sensing that line has already blurred, it’s time to consider what care could look like on your own terms.
Ready to find out what life feels like without the exhaustion of keeping it together? Call 866‑931‑6429 or visit Evoke Wellness at Cohasset to learn more about our opioid addiction treatment services in Cohasset, MA.
FAQs
Q: Do I have to check into rehab or can I do outpatient treatment?
A: Options range from full residential stays to outpatient therapy and medication-assisted treatment. We’ll match care to your life’s demands. Flexibility is a priority.
Q: I’ve got a good job and a family—does treatment even consider that?
A: Absolutely. High-functioning life roles often get overlooked. At Evoke Wellness, we design treatment plans that respect your work and family commitments.
Q: Will I have to stop everything and disrupt my life?
A: No. We offer partial hospitalization and intensive outpatient options—designed to let you keep your life moving forward while getting help.
Q: How do I know it’s not just stress or burnout?
A: If opioid use is involved in your emotional regulation—or if withdrawals happen when you pause—that’s a different pattern. Stress doesn’t cause physical cravings.
Q: I’m afraid of being judged if I go to treatment. Will people know?
A: Confidentiality is foundational. No one gets access to your medical decisions without permission. Treatment is a private step—one you can take while still looking the part of “normal.”